 |
de | fr | en Druckansicht ![]()
3R-Project 146-15
Validation of a novel cell-based approach to study thyroidal physiology: Reduction and/or replacement of experiments with rodents
Gerasimos P. Sykiotis
Service of Endocrinology, Diabetology and Metabolism, Lausanne University Hospital, 1011 Lausanne, Switzerland
gerasimos.sykiotis@chuv.ch
Keywords: braf; follicle; goiter; stem cells; thyroxin; replacement
Duration: 3 years Project Completion: 2019
Background and Aim
Hormones that are secreted by the thyroidal gland are necessary for embryonic development and for a proper functioning of the adult organism. Since the organ in mice is exceedingly small, weighing no more than 2mg, research on the thyroid has been traditionally conducted on rats, with the exception of genetic manipulations. However, in recent years, knockout (KO) murine models have been implemented and, owing to the size limitation, in necessarily large numbers per experimental group (n=8-12). Unfortunately, conventional (two-dimensional) thyrocytic lines of murine, rat or human origin are not representative models of the in-vivo situation, the reason thereof being that the specific functions of the organ depend upon the formation of anatomic units, namely, follicles, which are thyrocyte-lined spherical structures. Recently, protocols have been published that permit the generation of mature thyroidal follicles from murine and human embryonic stem (ES) cells (1-3). These protocols rely on the engineering of ES-cell lines that express transgenes encoding the transcription factors NKX2.1 and PAX8, which are central to thyrocytic specification (4). For a complete differentiation of the ES-cells into functional thyrocytes and the formation of follicles, an induction of NKX2.1- and PAX8-expression, followed by exposure to specific differentiation-promoting factors [such as activin and the thyroid-stimulating hormone (TSH)] and culturing in a three-dimensional (3D)-matrix, are requisite. The functionality of the resulting follicles is attested by their ability to capture and organify iodine for the synthesis of thyroidal hormones (1, 2). Furthermore, after transplantation into mice lacking a thyroid, such follicles can form functional thyroidal tissue in vivo and rescue the animals from otherwise lethal hypothyroidism (1).
Thus far, these protocols have been used to model the specification and differentiation of thyroidal cells, and to validate the importance of specific genetic and humoral factors in this process. However, the utility of the new cellular system as an alternative to animal models for the study of thyroidal physiology has not yet been put to the test. As a proof-of-concept, we will investigate whether the functional thyroidal follicles that are derived from murine ES (mES)-cells can be used to simulate the effects that are observed in murine KO or knock-in (KI) models of genes that are central to specific relevant pathways in thyroidal physiology, growth and/or oncogenesis, such as the Keap1/Nrf2 antioxidant-response pathway (5) and the BRAF-branch of the MAPK-pathway. The main goals are: (i) to ascertain whether a pharmacologically-mediated up- or down-regulation of a pathway of interest in thyroidal follicles that are differentiated from wild-type (for the specific pathway) endodermally-matured ES-cells can recapitulate the effects that are observed in the corresponding murine KO-models (genetic up- or down-regulation of the same pathway); and (ii) to ascertain whether thyroidal follicles that are differentiated from endodermally-matured ES-cells that have been genetically engineered before or after differentiation to up- or down-regulate a pathway of interest can recapitulate the observed effects in the corresponding murine KO or transgenic models of the same pathway (cellular KO/transgenic versus animal KO/transgenic).
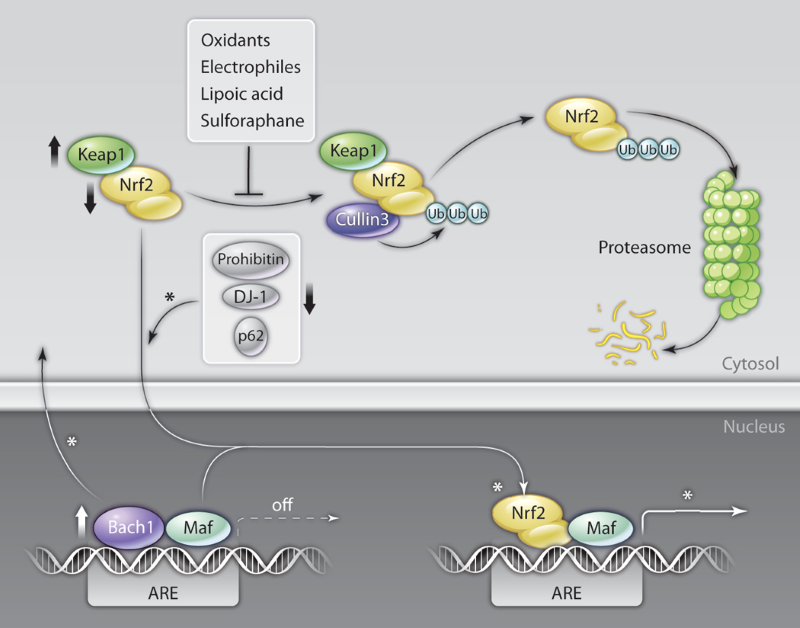
Figure 1: Scheme of the Keap1/Nrf2 antioxidant-response pathway. Under basal conditions, Nrf2 is targeted by Keap1 in the cytoplasm for Cullin3-mediated ubiquitination (Ub) and proteasomal degradation. Oxidative stress or specific compounds block the Keap1-mediated inhibition of Nrf2, thereby promoting an accumulation of the transcription factor in the nucleus and an induction of the transcription of its target genes by binding to antioxidant-response elements in their regulatory sequences.
Method and Results
Aim 1. Hypothesis: Thyroid-specific murine embryonic stem cells (ts-mES) can recapitulate the thyroid-specific phenotypes that are observed in the corresponding murine KO-models under basal and stressful conditions.We will combine the recently published 3D-follicle protocols with CRISPR/Cas9 gene-targeting or with lentivirus-mediated shRNA-expression to generate 3D-cultures of differentiated follicular cells with functional gains or losses in the Keap1/Nrf2 antioxidant-response system. We will characterize these follicles under basal conditions as well as under stressful ones (iodine treatment) and/or after a pharmacological manipulation of Nrf2-signalling (using the Nrf2-activator, CDDO, and the Nrf2-inhibitor, brusatol). Assayed parameters will include: (i) proper follicular organization; (ii) thyroid-specific expression of antioxidants at the gene and protein levels; and (iii) functional properties regarding iodide trapping, iodide organification and thyroid-hormone synthesis.These experiments will permit us to directly compare and contrast the molecular and biochemical phenotypes of mES-derived thyroidal follicles with those of thyroid-specific Nrf2- or Keap1-KO-mice (using PAX8-Cre-driven recombination), which we are creating and analyzing in parallel as part of an SNF-funded project. We expect to be able to model in vitro, either partially or fully, the in-vivo murine phenotypes.
Aim 2. Hypothesis: Thyroid-specific murine embryonic stem cells (ts-mES) can model experimental goitrogenesis and can recapitulate the thyroid-specific phenotypes that are observed in the corresponding murine models. To maximize the utility of the in-vitro model from a 3R-perspective, we will attempt to establish an in-vitro model of goitrogenesis using ts-mES-cells, and will compare the data thereby generated with the results of experimental goitrogenesis in our KO-models and in wild-type mice. To this end, ts-mES-cells will be induced to form thyroidal follicles in 3D-cultures and then subjected to different goitrogenic experimental conditions (low-iodine media, treatment with high doses of recombinant TSH, and/or anti-thyroid drugs in various combinations). The impact of genetic manipulation of the Keap1/Nrf2-pathway will also be assessed under these conditions.
Aim 3. Hypothesis: Thyroid-specific murine embryonic stem cells (ts-mES) that constitutively or conditionally express BRAF-V600E can model BRAF-V600E-mediated thyroidal oncogenesis and can recapitulate the phenotypes that are observed in the corresponding murine models. A papillary carcinoma is the most common form of thyroidal malignancy. In ~50% of cases, the tumours harbour activating mutations in BRAF, a serine/threonine kinase that transduces regulatory signals via the MAPK-cascade. The BRAF-V600E-mutation is the most common genetic aberration (>90%). We will explore whether the functional thyroidal follicles that are obtained from mES-cells that have been genetically engineered to conditionally express BRAF-V600E using a tetracycline-inducible system can reproduce most of the effects that are observed in the corresponding murine models in vivo. Specific measures will include: (i) BRAF-activity; ii) escape from proliferative arrest; (iii) morphological and architectural changes in the thyroidal follicles and the lumenal compartment; (iv) loss of cellular polarity; (v) signs of thyroidal dedifferentiation; (vi) changes that are consistent with an epithelial-to-mesenchymal transition; and (vii) genomic instability.
Conclusions and Relevance for 3R
We will characterize various molecular and morphological parameters in thyroidal follicles that have been derived from mES-cells under normal conditions and under the influence of different pharmacologically- and genetically-induced perturbations that are relevant to thyroidal physiology and pathologies (iodine deficiency or excess, goitrogenesis, oncogenesis). We will then compare the profiles of the mES-derived thyroidal follicles with data that have been gleaned from mice of the corresponding genotypes in the context of our ongoing SNF-funded project (31003A-153062-1) as well as with literature findings. These comparisons will permit us to directly validate (or refute) the utility of the new in-vitro model as a proxy, a screening assay and/or a complete replacement method for in-vivo studies on thyroidal physiology using KO-mice. If validated as an alternative method, the use of ES-cell-derived follicles will greatly reduce and largely replace experiments with wild-type and KO-mice in studies appertaining to thyroidal physiology. To promote the goals of 3R, all materials that are implemented and all knowledge that is gained will be made freely available to other investigators.
References
1. Antonica F, Kasprzyk DF, Opitz R, Iacovino M, Liao XH, Dumitrescu AM, Refetoff S, Peremans K, Manto M, Kyba M, Costagliola S (2012). Generation of functional thyroid from embryonic stem cells. Nature 491:66-71.
2. Ma R, Latif R, Davies TF (2013). Thyroid follicle formation and thyroglobulin expression in multipotent endodermal stem cells. Thyroid 23:385-91.
3. Ma R, Latif R, Davies TF (2015). Human embryonic stem cells form functional thyroid follicles. Thyroid 25:455-61.
4. De Felice M, Di Lauro R (2011). Minireview: Intrinsic and extrinsic factors in thyroid gland development: an update. Endocrinology. 152:2948-56.
5. Sykiotis GP, Bohmann D (2010). Stress-inducible cap’n’collar transcription factors in aging and human disease. Science Signaling. 122:re3.
| Letzte Änderung: 12.10.2018 |