 |
de | fr | en Druckansicht ![]()
3R-Project 124-10
Comparative in vitro and in vivo testing on biofilm formation on the surface of bone grafts
Martin Clauss1 and Andrej Trampuz2
1Kantonsspital Liestal, Orthopädie, 4410 Liestal, Switzerland
2CHUV, Infectious disease service, 1001 Lausanne, Switzerland
martin.clauss@ksli.ch, andrej.trampuz@chuv.ch
Keywords: orthopedics; replacement; infectiosity
Duration: 2 years Project Completion: 2013
Background and Aim
Infections associated with orthopaedic implants rarely occur, but represent one of the most devastating complications with high morbidity and substantial costs (1). These implant-associated infections are typically caused by micro-organisms that grow in biofilms (1). Extensive research has been performed in recent years to determine the propensity of medical devices to sustain biofilm formation (2). We recently established an in-vitro setting to analyse biofilm formation on bone grafts and bone graft substitutes (3), and showed in-vitro the importance to monitor (i) material properties (3), and (ii) incubation conditions (4) when investigating biofilm formation on bone grafts. Importantly, it remains unclear whether these in-vitro data are meaningful for in-vivo biofilm formation.
The planned experiment will compare the data of our in-vitro biofilm experiments on bone grafts with data from biofilms produced in-vivo in an established animal model for foreign body infections (5-7). In-vivo data obtained in the guinea-pig model can be directly transferred for predicting efficacy in humans (8), making this model an appropriate and validated tool to investigate implant-associated infections.
The aim of this project is (i) to compare in-vitro and in-vivo biofilm formation on the surface of calcium phosphate (CaP, Fig. 1) bone grafts, and (ii) to establish an in-vitro setting for biofilm formation to reduce the number of animals needed in preclincial trials for testing infect susceptibility of bone grafts in general.
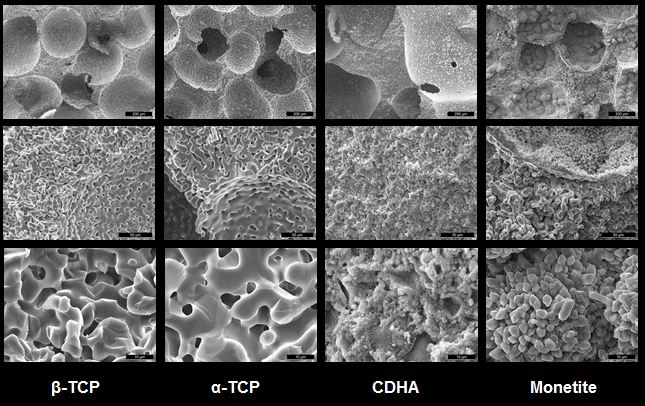
Figure 1: CaP bone grafts used for comparison: alpha tri-calcium phosphate (α-TCP), beta tri-calcium phosphate (β-TCP), calcium deficient hydroxyapatite (CDHA) and Monetite. The used bone grafts can be produced out of each other by means of thermal and chemical transformation (For further details see Bohner M 2000 Injury 31 Suppl 42 and Galea L 2008 Biomaterials 29).
Method and Results
In-vitro biofilm formation of staphylococcal strains on CaP bone grafts: CaP bone grafts will be incubated in pooled human serum. Then samples will be infected by inoculation with 1 x 105 colony-forming units (cfu) of either S. aureus ATCC 29213 (MSSA), S. aureus ATCC 43300 (MRSA) or S. epidermidis RP62A ATCC 35984 (MSSE). Samples with adjacent biofilm will be harvested at defined time points (4).
In-vivo biofilm formation of staphylococcal strains on CaP bone grafts: Biofilm will be formed in tissue cages in the back of guinea pigs. For this purpose four sterile polytetrafluorethylene (Teflon) tubes will be prefilled with CaP grafts and sterilised. They will then be implanted into the flanks of albino guinea pigs (Fig. 2).
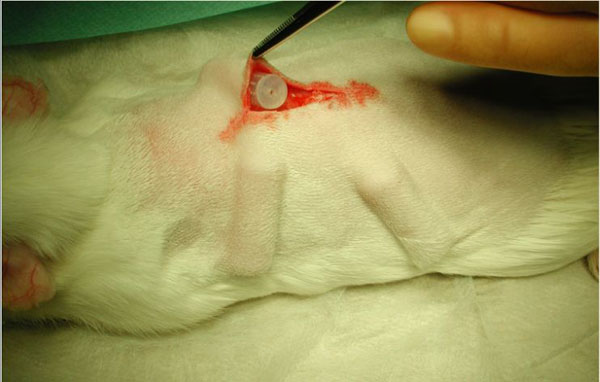
Figure 2: Guinea pig modell with ongoing implantation of tissue cages pre-filled with CaP bone grafts. (Courtesy of Prof. W. Zimmerli, Liestal)
These tissue cages, which have been prefilled with CaP grafts, will be infected by inoculation with 1 x 105 cfu of either S. aureus ATCC 29213 (MSSA), S. aureus ATCC 43300 (MRSA) or S. epidermidisRP62A ATCC 35984 (MSSE). Identical time intervals will apply to infecting the grafts in-vivo and in-vitro. The animals will be killed and CaP samples harvested.
Comparative biofilm analysis:
CaP bone grafts will be transferred to a 48-channel batch microcalorimeter (thermal activity monitor, model 3102 TAM III; TA Instruments, DE, USA) and Heat Flow measured at 37 ± 0.0001°C with a sensitivity of 200 nW for 24h. The microcalorimetry procedure has recently been described in detail (3). In brief, samples will be transferred to sterile 4 ml microcalorimeter ampoules pre-filled with 1 ml TSB, and transferred to the microcalorimeter.
Conclusions and Relevance for 3R
In-vitro biofim formation on bone grafts will be compared with in-vivo biofilm formation. It is hypothesized that in-vitro results can predict the in-vivo behaviour. The results should form a basis to develop a valid in-vitro screening test for biofilm formation on the surface of medical devices, helping to reduce the number of animals needed for definitive pre-clinical in-vivo tests.
References
1. Trampuz A, Osmon DR, Hanssen AD, Steckelberg JM, Patel R. Molecular and antibiofilm approaches to prosthetic joint infection. Clin Orthop Relat Res. 2003 Sep(414):69-88.
2. Harris LG, Richards RG. Staphylococci and implant surfaces: a review. Injury. 2006;37(2 SUPPL.).
3. Clauss M, Trampuz A, Borens O, Bohner M, Ilchmann T. Biofilm formation on bone grafts and bone graft substitutes. Comparison of different materials by a standard in vitro test and microcalorimetry. Acta Biomaterialia. 2010;6:3791-9.
4. Clauss M, Furustrand HU, Bizzini A, Trampuz A, Ilchmann T. Serum proteins influence biofilm formation on bone grafts – A microcalorimetrc in-vitro study comparing fresh, fresh-frozen and processed human and bovine spongiosa grafts Manuscript submitted 2011.
5. Zimmerli W, Waldvogel FA, Vaudaux P, Nydegger UE. Pathogenesis of foreign body infection: description and characteristics of an animal model. J Infect Dis. 1982 Oct;146(4):487-97.
6. Zimmerli W, Lew PD, Waldvogel FA. Pathogenesis of foreign body infection. Evidence for a local granulocyte defect. J Clin Invest. 1984 Apr;73(4):1191-200.
7. Zimmerli W. Experimental models in the investigation of device-related infections. J Antimicrob Chemother. 1993 May;31 Suppl D:97-102.
8. Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004 Oct 14;351(16):1645-54.
9. Furustrand Tafin, U., et al. Staphylococcal biofilm formation on the surface of three different calcium phosphate bone grafts: a qualitative and quantitative in vivo analysis. J Mater Sci Mater Med. 2015 March;26: 130-138.
| Letzte Änderung: 12.10.2018 |